 Stage 2: The Freshman Caregiver™
Stage 2: The Freshman Caregiver™
I am starting to help a family member or friend.
Who are you?
You’ve begun to help your family member on a regular basis, weekly, perhaps even a few times a week. Your duties range from errand-running and bill-paying to some assistance with hands-on care.
Your keyword: Find
–Find services that help.
–Find support that comforts.
–Find ways to enjoy your hobbies and interest.
Your Challenge
To discover solutions that work.
Your Purpose
This is your entry into the caregiving role. This is your time to experiment, to get your feet wet and see what works. This is your opportunity to learn how the health care industry works with, or in some cases, against you. Now is the time to shape your caregiving personality: What duties are you comfortable with? What duties make you uncomfortable? How well are you and your caree getting along? What situations would create overwhelming stresses for both of you? (To help you determine your caregiving personality, we’ve included information on how to create your Caregiving Mission Statement.)
This is also the time when you get a feel for the present and future budgets needed to provide the care your caree requires.
In addition, keep up with your hobbies and interests (you may be able only to keep the ones that you enjoy most), ensuring you have made a habit of spending time on your own, enjoying yourself.
As a “freshman caregiver,” what can you do?
1. Learn as much as you can about your caree’s illness, disease or condition.
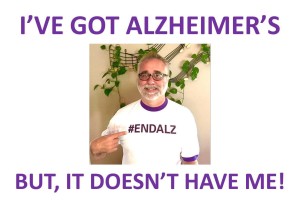
Consult the local branches or chapters of national organizations such as The Arthritis Foundation, the Alzheimer’s Association, The Cancer Society. What does the future hold for you and your caree?
2. Learn how to provide proper care from health care professionals or from health care videos, manuals or books.
If your caree is hospitalized or receives short-term therapy at a nursing home, ask the staff to show you proper caregiving techniques: lifting, transfers, bathing. If you can, record the therapy sessions so you can refer to your videos when you’re providing the care at home. Or, search the Internet, including YouTube.com, for hands-on care information and tutorials.
It’s very difficult to provide care when you are unsure of what you’re doing. You’ll feel much better when you’re confident of your skills.
3. Join a support group–online or in your community.
It’s so isolating to be a caregiver! Support groups will hook you up with others in similar situations; often, you’ll learn of community resources and options from other caregivers that you were not aware of.
4. Count on regular breaks from caregiving.
Plan for regular breaks–an hour daily, an afternoon weekly, or a day monthly–whatever you can manage. Enlist the help of relatives and community services (such as a volunteer group at your local church) so you can take time off regularly. Relatives can help in many ways–through financial support, social support (calling the caree regularly just “to talk”) as well as respite support.
5. Rely on help from community organizations.
Meals on Wheels, home care agencies and day care centers, to name just a few, may offer services that your caree needs.
Contact your local Area Agency on Aging for a listing of services and organizations in your community. Visit your local medical equipment supply store to find devices and gadgets that enhance your caree’s abilities–and independence from you. Remember, allowing the help of others is a sign of strength.
In addition, ask about local, state or federal programs (like the Veterans Administration’s Aid and Attendant Care Program) that might provide financial assistance for you and/or your caree. As your caree’s care needs increase, so will the costs associated with his or her care. Understanding what programs can help, in addition to understanding what your caree can afford, will help you plan appropriately for the future.
6. Create your rhythm of helping.
You’ll want to find your flow–the rhythm of what you do, what other family members do, what you hire to get done and what your caree does. Keeping the rhythm, which will change and ebb and flow, helps you keep what’s important to you (activities, career, relationships).
7. Keep your caree’s wishes in mind.
When appropriate, ask for his or her input and ideas. Does your caree still feel good about living at home? What does your caree fear or dread? (These are also good questions to ask yourself!)
You may disagree with your caree’s lifestyle choices. You may be incredibly exasperated by your caree’s inability to accept help or make good decisions. Vent your frustations in your journal and to your support group. It’s your caree’s life, which means you want to respect his or her decisions.
If your caree suffers from a cognitive impairment, you’ll want to step in and ensure your caree’s safety. If you struggle to keep your caree safe, consider hiring a geriatric care manager who can help put solutions in place. (You can learn more about geriatric care managers and locate one near your caree here: www.caremanager.org.)
8. Reflect the changes in your journal.
How do you feel now? What are your concerns? Fears? What outcomes are you working toward? What losses have you noticed during this period? What changes in the relationship cause you to feel sad? What changes have given you comfort?
9. Start a second journal that you use to detail your caree’s needs and your caregiving responsibilities.
Note any changes in your caree’s health and condition so that you can confidently discuss your concerns during physician appointments. Use your journal as a caregiving manual, which will help when others step in to provide care. Continue to chronicle your caregiving journey in your first journal. What causes you to mourn?
10. Create a spreadsheet that details your caree’s medical history, medications, hospitalizations, treatments and changes in medical status.
A searchable document, like a spreadsheet, will be handy throughout your caregiving experience. You’ll be able to easily find details relating to important information, such as previous hospitalizations, medication changes and lab results.
11. Create the habit of regularly holding family meetings.
And, if you and your caree share a household with other family members (including children), consider creating House Rules. Rules for the household include:
–Who does what, how and when;
–Guidelines for fights, fun, and festivals (celebrations);
–Schedule of meetings and their purposes;
–Expectations in regard to support, engagement and participation.
12. Manage the money: Develop a budget, keep track of expenses, set up a filing system for bills and receipts.
Keep your caree’s expenses separate from yours and your family’s. Keep track (and receipts) of any of your caree’s bills that you pay. If you’re overwhelmed, consider having a professional, like a financial planner or bank trust officer, oversee your caree’s financial situation, including paying bills.
13. Start a Solutions Fund so you can hire solutions.
The account funds solutions for boredom, breaks and back-up plans. Contribute a monthly amount; allow yourself flexibility in how you use the monthly budget. Use the fund for your caree, for the house, for you.
Use the Solutions Fund for your caree to hire services such as home health, adult day or to purchase games from Marbles the Brain Store or products from The Alzheimer’s Store or activities from eNASCO.
Use the fund for your house (or your caree’s) to hire cleaning service, lawn maintenance, snow removal. The fund buys you services from a counselor or life coach, or for pampering services, adult education classes and activities.
Ask family members to contribute to your Solutions Fund.
14. Have back-up plans and then back-up plans for your back-up plan.
Ask yourself, “What if…” and then create a plan to manage the “What if’s.” If it can happen, most likely it will. Be ready with a plan. A geriatric care manager can be invaluable in developing your back-up plans. (Learn more about geriatric care managers and locate one near your caree.)
15. Help yourself, especially if your caree refuses help.
You may find great resources to help your caree, only to be shut down by a stubborn caree. As you spend more time with your caree, you’ll have less time to keep up with your responsibilities. Hire out services to help you, like housecleaning and lawn maintenance, as often as you can. Even if you can only afford a housecleaning service once a year, do it. And, do it when it will help you most.
In addition, keep up-to-date on community resources and providers. Although your caree may refuse help now, a day may come when you’ll need to step in with help.
16. Build your own paradise of privacy.
Call a spare bedroom or a corner in the basement your own. Add your favorite things (books, chocolate, candles, scrapbook, journal, music, TV, videos, photography, family photos) to make the space a retreat you love to use.
17. You are, and will continue to be, your caree’s most important health care provider.
You have critical knowledge of your caree’s health. More than anyone, you know your caree best, which means you are your caree’s best advocate.
18. Continue to maintain your healthy lifestyle.
Take note when the stress causes too much comfort food or too few walks. One of your best defenses against the impact of stress is a healthy lifestyle.
19. An apple a day…
What’s your apple in this stage? What helps you to feel good on a daily basis? Enjoy your apple every day.













Recent Comments